Rudra Narayan Saha
Department of Textile Technology
Dr B R Ambedkar National Institute of Technology Jalandhar
Email Id: rudenarayansaha37469@gmail.com
Introduction
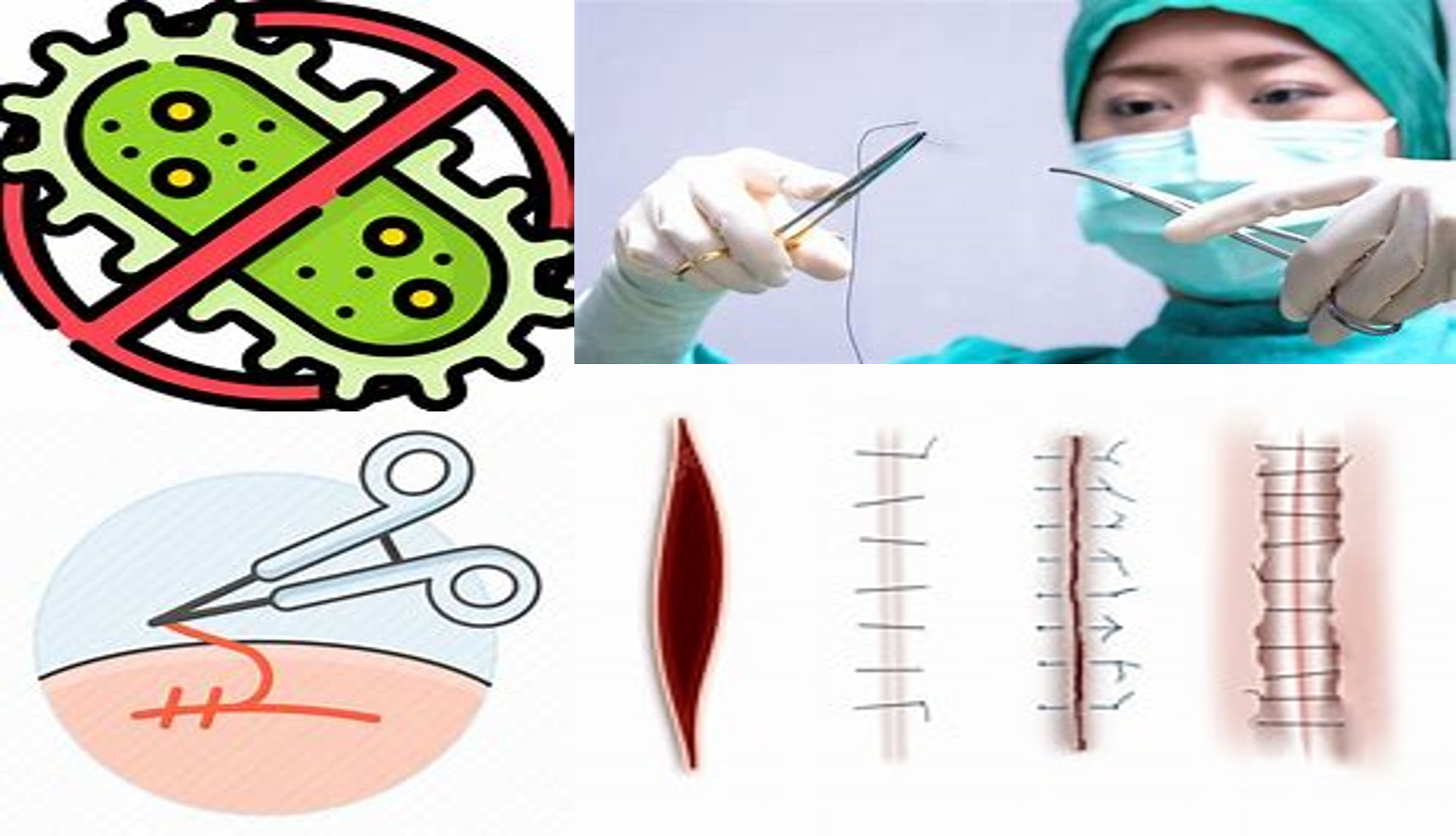
Surgical sutures, referred to as stitches or stitches, are medical devices used to approximate the edges of wounds following surgery or join tissues together. Sutures are mainly classified as absorbable (e.g. catgut, Polyglactin) and non-absorbable (silk, nylon). It is categorized by its structure into monofilament and multifilament or braided and further as natural (catgut, silk) or synthetic (PGA, polyglactin, polyester) suture by origin (Bennett, 1988). All Braided suture materials, including natural sutures like silk, create high friction and drag, causing tissue trauma and providing ideal conditions for bacterial colonization due to gaps between strands and capillarity. Due to their high capillarity and propensity to collect debris and bacteria, foreign protein-based silk sutures cause severe inflammatory reactions, hinder healing, and raise the risk of infection. Medical device-related infections are difficult to cure and frequently call for prolonged hospital stays and additional therapies. Lowering the bacterial adhesion on these devices can lower infection rates. Approximately 17% of hospital-acquired infections are caused by Surgical site infections and extreme cases result in death from sepsis or another complication. It is challenging to get rid of germs on sutures, and the creation of biofilms and bacterial proliferation on multifilament sutures increases the risk of infection (Ming et al., 2008; Stephen et al., 2002).
Several studies indicate that sutures significantly increase susceptibility to infection, wound disruption, and chronic sinus formation in surrounding tissues. Bacteria can adhere to medical devices during surgery, leading to a high risk of contamination. Reducing bacterial presence at surgical sites could lower the frequency of infections. The physical structure of sutures has been identified as a contributing factor to surgical infections, with intrinsic surface roughness and capillarity of braided sutures increasing the risk of wound infection, as reported in reputed journals. Researchers have proposed coating the surface of sutures with antibacterial agents to prevent the development of bacterial colonies on medical devices without compromising their mechanical properties. Numerous studies since the early 1980s have documented physical and chemical protocols for developing antibacterial sutures (Bhouri et al., 2022). Therefore, the primary approach to treating suture-associated SSI is to coat the suture surface with antibacterials or antifungals that restrict bacteria growth while maintaining mechanical and morphological characteristics. Due to their low toxicity, biodegradability, and biocompatibility, chemicals like triclosan, N-halamines, natural substances like chitosan & and grapefruit seed and olive leaf extract, and metals like silver and its nanoparticles, zinc, titanium, copper have received the majority of study attention (Seydibeyoglu & Isik, 2020; Umair et al., 2015).
Antibacterial finish
An antibacterial or antimicrobial finish is a chemical treatment applied to textiles to inhibit the growth and proliferation of microorganisms, such as bacteria, fungi, and viruses. This finish helps to reduce odors, stains, and degradation of the fabric, thereby enhancing the hygiene,
durability, and overall performance of the textile products. Antibacterial finishes are used in a variety of applications, including medical textiles, sportswear, home furnishings, and protective clothing (Di Martino, 2022).
An ideal antibacterial finish for textiles should meet several key criteria to ensure maximum effectiveness and safety (Nayak & Padhye, 2015; Petrova et al., 2021):
- It should be effective against a broad spectrum of microorganisms.
- It must exhibit low toxicity to humans, avoiding allergic reactions or irritation. • It should not harm the skin’s resident non-pathogenic bacteria, which are vital for skin health by lowering surface pH and producing antibiotics to inhibit pathogenic bacteria. • The finish must comply with governmental regulations and have a minimal environmental impact.
- Sutures treated with the antibacterial finish should pass compatibility tests (cytotoxicity, irritation, and sensitization) before being marketed.
- It must be cost-effective and eco-friendly.
Most antibacterial agents used in the medical and textile industries operate through a controlled release or leaching mechanism. Leaching antibacterials are not chemically bonded to the textile fibers; their antibacterial activity is due to the gradual and sustained release of the active substance from the textile material into the environment in the presence of moisture. However, to maintain the effectiveness of the finish, the concentration must not fall below the minimum inhibitory concentration (MIC). Some antibacterial finishes based on a controlled release mechanism contain active substances that are leachable in water. The primary advantage of these chemicals is their ability to be regenerated under suitable conditions (Nayak & Padhye, 2015). Different types of antibacterial finishes applied in medical textiles are described in the following section.
Triclosan
2,4,4′-Trichloro-2′-hydroxydiphenyl ether (triclosan) is an antimicrobial agent effective against various bacterial species, with a minimum inhibitory concentration (MIC) of less than 10 ppm. It functions by blocking lipid biosynthesis and inhibiting microbial growth. Unlike most cationic biocides used in textiles, triclosan remains non-ionized in solution. Its antimicrobial effect is achieved through the gradual migration of triclosan to the fabric surface during use. The durability of triclosan can be enhanced by incorporating it into the hydrophobic cavity of β-cyclodextrins to form an inclusion complex (Lu et al., 2001).
Triclosan has been utilized for its antiseptic properties for many years in products such as toothpaste and soap and has an established safety profile. It has been employed to coat various sutures, including braided polyglactin 910 (Vicryl Plus), poliglecaprone 25 (Monocryl Plus), and polydioxanone (PDS Plus), and received approval from the US Food and Drug Administration in 2002. Both in vitro and in vivo studies have demonstrated the efficacy of triclosan-coated sutures in eliminating bacteria associated with surgical site infections (SSIs) and preventing colonization of suture material. One study reported a 66% reduction in bacterial colonization with triclosan-coated sutures (Ahmed et al., 2019; Ming et al., 2008; Stephen et al., 2002).
Metal compounds
Several heavy metals, either in their free state or as compounds, are toxic to microbes at very low concentrations, killing them by binding to inactivating intracellular proteins. Silver (Ag) is the most widely used antimicrobial agent in textiles due to its non-toxic and non-carcinogenic nature, with a minimum inhibitory concentration (MIC) of 0.05 to 0.1 mg/l against Escherichia coli (De Simone et al., 2014; Rai et al., 2009). The antimicrobial activity of metal nanoparticles is attributed to their small particle size and high specific surface area, which increases the release of metal cations, enhancing their biocidal effectiveness. Recently, there has been significant interest in using inorganic nanostructured materials with strong antimicrobial properties for textile applications. These materials include titanium dioxide (TiO₂) nanoparticles, metallic and non-metallic TiO₂ nanocomposites, titania nanotubes (TNTs), silver-based nanostructured materials, gold nanoparticles, zinc oxide nanoparticles and nanorods, copper nanoparticles, carbon nanotubes (CNTs), liposome-loaded nanoparticles, and metallic and inorganic dendrimer nanocomposites (Ruparelia et al., 2008; Yadav et al., 2006).
N-halamines
N-halamines have demonstrated stable, potent, and durable biocidal activity against a broad spectrum of microbes. An N-halamine compound contains one or more nitrogen-halogen covalent bonds, formed by the halogenation of imide, amide, or amino groups (Cerkez et al., 2012). Its mode of action involves the release of positive chlorine from the N-halamine structure, which penetrates the cell wall and binds to suitable receptors within the cells, inhibiting cell metabolism and causing microbial death. N-halamine biocides kill microorganisms directly by releasing positive chlorine into the system. N-halamine moieties have been introduced through various methods to produce antibacterial cellulose, nylon, polyester (PET), and stainless steel. The application of N-halamine results in a significant amount of absorbed chlorine (or other halogens) remaining on the fabric’s surface in addition to the covalently bonded N-halamines. These halogens can produce unpleasant odors and cause fabric discoloration. To remove the residual halogens from the fabrics, a reduction process using sodium sulfite can be employed (Sun & Sun, 2001; Umair et al., 2015).
PAMBM (poly[(aminoethyl methacrylate)-co-(butyl methacrylate)])
An amphiphilic polymer, poly[(aminoethyl methacrylate)-co-(butyl methacrylate)] (PAMBM), exhibits significant antimicrobial activity against both Gram-positive bacteria (S. aureus: MIC = 12.5 μg/mL) and Gram-negative bacteria (E. coli: MIC = 25 μg/mL). PAMBM acts as a bactericidal agent, similar to natural antimicrobial peptides (AMPs), due to its ability to disrupt bacterial membranes, leading to leakage of cytoplasmic contents and subsequent cell death. In contrast, triclosan functions as a bacteriostatic agent at lower concentrations, inhibiting bacterial growth and reproduction rather than killing bacteria. This fundamental difference in mechanism underscores the potential advantage of PAMBM over triclosan as an active component in antimicrobial suture coatings (Li et al., 2012; Melo et al., 2009) .
Chitosan
Chitosan, a deacetylated derivative of chitin and the second most abundant polysaccharide on Earth after cellulose, is derived from the shells of crustaceans like shrimp, crab, and lobster. It is renowned for its antimicrobial properties against a variety of bacteria and fungi due to its polycationic nature (Fu et al., 2011). The effectiveness of chitosan depends on factors such as molecular weight, degree of deacetylation, pH, and temperature. Additionally, chitosan is non toxic, biocompatible, and biodegradable, with a minimum inhibitory concentration (MIC) of 0.05–0.1% against many bacterial species (Lim & Hudson, 2003). While chitosan has been used to impart antimicrobial properties to cotton, wool, and silk fabrics, its weak adhesion to cellulosic materials leads to gradual leaching during laundering. To address this, chitosan has been crosslinked to cotton using chemicals such as dimethylol dihydroxy ethylene urea (DMDHEU) and polycarboxylic acids (Das et al., 2023a; Zhang et al., 2003).
Method to apply the antibacterial finishes
The pad–dry–cure process is the most commonly used conventional method for applying antimicrobial finishes to fabrics, where a coating is applied to the fabric surface. Antibacterial agents such as chitosan, triclosan, and zinc oxide have been applied to both natural and synthetic textiles using this method. Other techniques for applying antibacterial finishes include microencapsulation, enzyme immobilization, treatment with resins or crosslinking agents, layer-by-layer deposition, nanocoating, and polymerization grafting (Das et al., 2023b; Dubas et al., 2006; Edwards et al., 2012; Rajendran et al., 2010; Sun & Sun, 2002; Xing et al., 2007). Unlike conventional methods, many of these alternative approaches introduce antibacterial activity at the micro or nano level, preserving the fabric’s bulk properties. These methods enhance the functionality of textiles while minimizing impacts on fabric strength, feel, handle, or comfort.
Evaluation process of antibacterial finishes
Agar diffusion test
Textile samples are placed in intimate contact with agar plates, which contain a growth medium for culturing microorganisms. After incubation at 37°C for 18–24 hours, bacterial growth is assessed underneath and around the fabric edges. Antimicrobial activity is indicated by the absence of bacterial growth directly under the fabric and the formation of a clear zone of inhibition around the sample, reflecting the potency and diffusion rate of the antibacterial agent(Das et al., 2023a, 2023b).
Japanese Industrial Standard Assay (JIS Z 2801)
A suspension of S. aureus (105cells/mL) in sterile phosphate-buffered saline (PBS) is prepared and placed into a chromatography sprayer. Disc samples with varying amounts of antibacterial agents are sprayed equally and evenly with the bacterial solution. Sterile PBS is applied to each sample surface, diluted, and spread onto Mueller Hinton agar plates. The plates are incubated at 37°C for 24 hours, and viable colonies are counted. All colony counts are converted into colony-forming units per mL (CFU/mL), and the bactericidal activity is assessed by comparing the colony growth on the treated samples to that on control samples without coating (Li et al., 2012).
Conclusion
The ongoing development and refinement of antibacterial finishes for surgical sutures are crucial for enhancing the safety and effectiveness of medical devices and reducing infection rates and improving patient outcomes. Effective finishes inhibit bacterial growth while maintaining the sutures’ mechanical properties and biocompatibility. Promising agents include metals like silver, N-halamines, and PAMBM, with chitosan offering a biodegradable alternative, though its adhesion needs improvement. Various application methods, from traditional pad-dry-cure to advanced techniques like nanocoating and polymer grafting, integrate antibacterial properties without degrading fabric quality. Efficacy and safety are assessed through rigorous testing, such as the AATCC-147 and JIS Z 2801 assays. Continued research and innovation in antibacterial finishes will be essential for overcoming current limitations and addressing the evolving challenges in surgical care.
References
Ahmed, I., Boulton, A. J., Rizvi, S., Carlos, W., Dickenson, E., Smith, N. A., & Reed, M. (2019). The use of triclosan-coated sutures to prevent surgical site infections: A systematic review and meta-analysis of the literature. BMJ Open, 9(9), 1–12. https://doi.org/10.1136/bmjopen-2019-029727
Bennett, R. G. (1988). Selection of wound closure materials. Journal of American Academy of Dermatology, 18(4), 619–637.
Bhouri, N., Debbabi, F., Merghni, A., Rohleder, E., Mahltig, B., & Ben Abdessalem, S. (2022). New manufacturing process to develop antibacterial dyed polyethylene terephthalate sutures using plasma functionalization and chitosan immobilization. Journal of Industrial Textiles, 51(4), 6353S-6376S.
Cerkez, I., Kocer, H. B., Worley, S. D., Broughton, R. M., & Huang, T. S. (2012). N halamine copolymers for biocidal coatings. Reactive and Functional Polymers, 72(10), 673–679. https://doi.org/10.1016/j.reactfunctpolym.2012.06.018
Das, P., Roy, M. D., & Ghosh, S. (2023a). Hydrophobicity and antibacterial property of silica sol-chitosan-HDTMS treated silk fabric. Indian Journal of Fibre & Textile Research, 48(December), 442–449. https://doi.org/10.56042/ijftr.v48i4.7651
Das, P., Roy, M. D., & Ghosh, S. (2023b). Study on the Hydrophobicity and Antibacterial Activity of Silica Sol-Chitosan-HDTMS Treated Cotton Fabric Dipped in an Aquas Media. Tekstilec, 66(0), 1–14. https://doi.org/10.14502/tekstilec.65.2022094
De Simone, S., Gallo, A. L., Paladini, F., Sannino, A., & Pollini, M. (2014). Development of silver nano-coatings on silk sutures as a novel approach against surgical infections. Journal of Materials Science: Materials in Medicine, 25(9), 2205–2214. https://doi.org/10.1007/s10856-014-5262-9
Di Martino, P. (2022). Antimicrobial agents and microbial ecology. AIMS Microbiology, 8(1), 1–4. https://doi.org/10.3934/microbiol.2022001
Dubas, S. T., Kumlangdudsana, P., & Potiyaraj, P. (2006). Layer-by-layer deposition of antimicrobial silver nanoparticles on textile fibers. Colloids and Surfaces A: Physicochemical and Engineering Aspects, 289(1–3), 105–109.
Edwards, J. V., Prevost, N. T., Condon, B., French, A., & Wu, Q. (2012). Immobilization of lysozyme-cellulose amide-linked conjugates on cellulose I and II cotton nanocrystalline preparations. Cellulose, 19(2), 495–506. https://doi.org/10.1007/s10570-011-9637-5
Fu, X., Shen, Y., Jiang, X., Huang, D., & Yan, Y. (2011). Chitosan derivatives with dual antibacterial functional groups for antimicrobial finishing of cotton fabrics. Carbohydrate Polymers, 85(1), 221–227. https://doi.org/10.1016/j.carbpol.2011.02.019
Li, Y., Kumar, K. N., Dabkowski, J. M., Corrigan, M., Scott, R. W., Nüsslein, K., & Tew, G. N. (2012). New bactericidal surgical suture coating. Langmuir, 28(33), 12134–12139. https://doi.org/10.1021/la302732w
Lim, S. H., & Hudson, S. M. (2003). Review of chitosan and its derivatives as antimicrobial agents and their uses as textile chemicals. Journal of Macromolecular Science – Polymer Reviews, 43(2), 223–269. https://doi.org/10.1081/MC-120020161
Lu, J., Hill, M., Ood, M., Tonelli, A., Grreson, D., Horton, J., Orndroff, P., & Harndon, A. (2001). Formation of antibiotic, biodegradable polymers by processing with Irgasan DP300R (triclosan) and its inclusion compound with β‐cyclodextrin. Journal of Applied Polymer Science, 82(2), 300–309. papers2://publication/uuid/404787CF-F21A-44F7- A366-D80E11715D6C
Melo, M. N., Ferre, R., & Castanho, M. A. R. B. (2009). Antimicrobial peptides: Linking partition, activity and high membrane-bound concentrations. Nature Reviews Microbiology, 7(3), 245–250. https://doi.org/10.1038/nrmicro2095
Ming, X., Rothenburger, S., & Nichols, M. M. (2008). In vivo and in vitro antibacterial efficacy of PDS plus (polidioxanone with triclosan) suture. Surgical Infections, 9(4), 451–457. https://doi.org/10.1089/sur.2007.061
Nayak, R., & Padhye, R. (2015). Antimicrobial finishes for textiles. In Functional Finishes for Textiles: Improving Comfort, Performance and Protection. Woodhead Publishing Limited. https://doi.org/10.1533/9780857098450.2.361
Petrova, L. S., Yaminzoda, Z. A., Odintsova, O. I., Vladimirtseva, E. L., Solov’eva, A. A., & Smirnova, A. S. (2021). Promising Methods of Antibacterial Finishing of Textile Materials. Russian Journal of General Chemistry, 91(12), 2758–2767. https://doi.org/10.1134/S1070363221120549
Rai, M., Yadav, A., & Gade, A. (2009). Silver nanoparticles as a new generation of antimicrobials. Biotechnology Advances, 27(1), 76–83.
Rajendran, R., Balakumar, C., Ahammed, H. A., Jayakumar, S., Vaideki, K., & Rajesh, E. M. (2010). Use of zinc oxide nano particles for production of antimicrobial textiles. International Journal of Engineering, Science and Techbology, 2(1), 202–208. https://doi.org/10.1016/j.matlet.2019.126562
Ruparelia, J. P., Chatterjee, A. K., Duttagupta, S. P., & Mukherji, S. (2008). Strain specificity in antimicrobial activity of silver and copper nanoparticles. Acta Biomaterialia, 4(3), 707–716. https://doi.org/10.1016/j.actbio.2007.11.006
Seydibeyoglu, E. A., & Isik, A. (2020). Effect of Natural Antimicrobial Agents on the Characteristics of Surgical Sutures. Dokuz Eylul University Faculty of Engineering Journal of Science and Engineering, 22(64), 11–20.
Stephen, R., Daniel, S., Shubhangi, B., & Daniel, B. (2002). In Vitro Antimicrobial Evaluation of Coated VICRYL* Plus Antibacterial Suture (Coated Polyglactin 910 with Triclosan) using Zone of Inhibition Assays. SURGICAL INFECTIONS, 3, 79–87. https://doi.org/10.1089/sur.2002.3.s1
Sun, Y., & Sun, G. (2001). Novel regenerable N-halamine polymeric biocides. II. Grafting hydantoin-containing monomers onto cotton cellulose. Journal of Applied Polymer Science, 81(3), 617–624. https://doi.org/10.1002/app.1477
Sun, Y., & Sun, G. (2002). Durable and regenerable antimicrobial textile materials prepared by a continuous grafting process. Journal of Applied Polymer Science, 84(8), 1592– 1599. https://doi.org/10.1002/app.10456
Umair, M. M., Jiang, Z., Ullah, N., Safdar, W., Xie, Z., & Ren, X. (2015). Development and characterisation of antibacterial suture functionalised with N-halamines. Journal of Industrial Textiles, 46(1), 59–74. https://doi.org/10.1177/1528083715573279
Xing, Y., Yang, X., & Dai, J. (2007). Antimicrobial finishing of cotton textile based on water glass by sol-gel method. Journal of Sol-Gel Science and Technology, 43(2), 187–192. https://doi.org/10.1007/s10971-007-1575-1
Yadav, A., Prasad, V., Kathe, A. A., Raj, S., Yadav, D., Sundaramoorthy, C., & Vigneshwaran, N. (2006). Functional finishing in cotton fabrics using zinc oxide nanoparticles. Bulletin of Materials Science, 29(6), 641–645.
Zhang, Z., Chen, L., ji, J., Huang, Y., & Chen, D. (2003). Antibacterial Properties of Cotton Fabrics Treated with Chitosan. Textile Research Journal, 73(12), 1103–1106. https://doi.org/10.1177/004051750307301213
About the Author: Rudra Narayan Saha is a graduate of Govt. College of Engg. & Textile Technology, Berhampore, West Bengal, where he earned his degree in Textile Technology. He also holds a Master's degree in Textile Engineering from GCETTB. Rudra N Saha specialises in the education of weaving and textile testing section. He is currently conducting research at NIT Jalandhar, focusing on advancements in medical textiles.
Account Sale Account Catalog
Buy accounts Find Accounts for Sale
website for buying accounts ready-made accounts for sale
verified accounts for sale https://top-social-accounts.org/
account exchange service https://accounts-offer.org/
account selling platform https://accounts-marketplace.xyz/
online account store https://accounts-marketplace.live/
account trading platform https://accounts-marketplace.online
account trading platform https://accounts-marketplace-best.pro
facebook ad account buy https://buy-adsaccounts.work
facebook ad account for sale https://buy-ad-accounts.click
buy a facebook account https://buy-ad-account.top
facebook account buy https://buy-ads-account.click/
facebook ads accounts buy a facebook account
buy facebook ads account buy fb account
facebook ads accounts facebook account buy
facebook bm account buy https://verified-business-manager-for-sale.org
buy tiktok ad account https://tiktok-ads-account-buy.org
tiktok ads account for sale tiktok ads agency account
buy tiktok ad account https://tiktok-agency-account-for-sale.org
buy tiktok ads account https://tiktok-ads-agency-account.org